With more people taking charge of their health, home health monitoring devices have become everyday essentials. Whether you’re managing a chronic condition like diabetes or hypertension, caring for someone at home or simply starting to get active, these devices make it easier to track health and spot early warning signs.
Here’s a simple guide to the most common devices.
Body Mass Index (BMI) can give a snapshot of your overall health. You can manually calculate your BMI with online calculators or this formula: BMI = weight (kg) ÷ [height (m)]²
You can also use BMI machines that measure your weight and height and calculate your BMI accordingly.
| If your BMI is… | Then… |
| Below 18.5 | Your weight is low. You may have nutritional deficiencies and a risk of osteoporosis. |
| 18.5 – 23.0 | You are in the healthy range. |
| Above 23.0 | You are in the high range. You have a higher risk of diabetes, high blood pressure and heart disease. |
Do note that BMI is a helpful starting point, but it doesn’t distinguish between muscle and fat. That’s why active individuals or athletes may have a higher BMI despite being healthy.
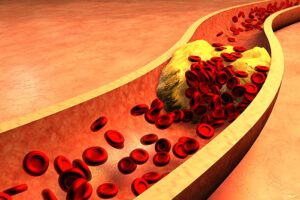
Blood pressure (BP) monitors are one of the most important tools for people with hypertension, a condition that often shows no symptoms. Home BP readings help you and your doctor understand how well your condition is controlled.
Understanding your BP reading:
- Systolic (top number): Pressure when your heart beats
- Diastolic (bottom number): Pressure when your heart relaxes
A reading above 140/90 mmHg repeatedly may indicate hypertension. People with diabetes or kidney issues may need to aim for below 130/80 mmHg.
There are two main types of BP monitors:
- Automatic BP monitors: Most user-friendly for home use
- Aneroid/manual monitors: Usually for trained professionals
Blood glucose (BG) monitors help individuals with diabetes track how food, activity and medication affect their sugar levels. Regular testing helps you understand how well-controlled the condition is and guides your doctor in adjusting treatment. It also prevents complications such as nerve damage, kidney issues and vision problems.
Worth noting is that BG monitors are preferable to urine glucose tests as they are faster and more sensitive to sugar in the blood. However, when using them, it is important to ensure the test strips are not expired and to take note of the brand’s safety and usage guidelines.
Health monitoring devices aren’t just for people with existing conditions. They are also helpful for:
- Seniors, or anyone with a higher risk of hypertension and diabetes
- People on weight-loss or fitness journeys
- Pregnant women, especially those at risk of gestational hypertension or diabetes
Ultimately, these devices empower you to catch small changes early, before the small signs become serious conditions.
Blood pressure and blood glucose monitors are available at FairPrice Online. You can also visit your nearest Unity outlet to check out the range of reliable devices, from blood pressure monitors to body composition scales.
For an even clearer picture of your health, drop by our Active Living Zone in selected stores. These zones are equipped with Tanita body composition analysers, which help you measure indicators such as BMI, body fat percentage and muscle mass in just a few minutes. Our pharmacists can also guide you through your Tanita result slip and offer advice tailored to your needs.
Need more help? Speak with a friendly Unity pharmacist on duty for guidance on choosing the right device for your needs, so you can take charge of your health with confidence!